

Pneumonia in seniors is a complex respiratory condition that presents unique challenges as people age. Understanding how it develops, who is most affected, and the best approaches for minimizing the dangers are crucial steps toward effective management. Seniors often face weakened immune systems and underlying health issues, making pneumonia more difficult to diagnose and treat, with potentially serious consequences if not managed carefully. Recognizing subtle symptoms, identifying risks, and approaching care systematically can make a significant difference in health outcomes for older adults.
An informed approach to senior pneumonia goes beyond basic awareness; it involves recognizing environmental triggers, seasonal patterns, and common misconceptions around risk factors. While many think of pneumonia as just another cold or flu, the impact on seniors can be much more serious, with longer recovery times and increased complications. Preventing pneumonia in older adults and caring for those already affected often requires a blend of medical oversight, personal vigilance, and community support.

The risks associated with pneumonia in Australian seniors are shaped by several factors—notably, age, comorbidities like diabetes or heart disease, and seasonal influenza patterns. Data from the Australian Institute of Health and Welfare indicate higher hospitalization rates for pneumonia among adults aged 65 and over, particularly during winter, underlining how environmental and physiological vulnerabilities converge.
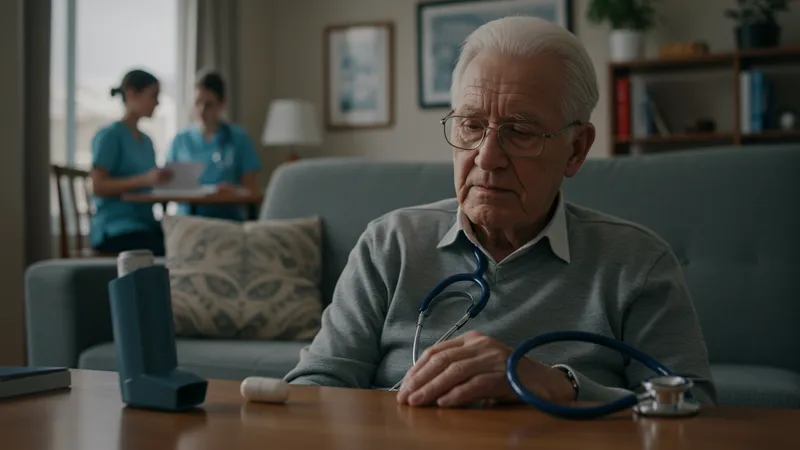
One notable benefit of a structured care strategy is early detection, which is often complicated by atypical symptoms in older adults. Unlike younger populations who may develop typical respiratory issues, seniors sometimes show confusion, reduced mobility, or general weakness, making it essential for caregivers and healthcare professionals to use thorough assessment and tailored interventions.
Comparing pneumonia care models across Australia, initiatives such as home health nurse visits and telemedicine services for seniors have demonstrated promising results for both prevention and rehabilitation. These programs facilitate regular check-ins, medication adherence, and post-hospitalization monitoring, all of which are linked to lower rates of pneumonia-related complications.
For families and caregivers, an in-depth understanding of available resources can make a significant difference. Accessing dedicated lung health organizations, reliable vaccination information, and professional guidance equips them to respond quickly to signs of illness while reducing the likelihood of severe outcomes. Learning from actual Australian support systems highlights how prepared communities can alter the trajectory of pneumonia in the elderly.
While these are the key touchpoints for understanding risks and care in senior pneumonia, the deeper details reveal even more valuable insights ahead—especially regarding how risk factors interplay and how best to support recovery in the Australian context.
Several interconnected risk factors amplify the likelihood and severity of pneumonia among seniors in Australia. Age remains the primary influence, as physiological defenses naturally decline, making the respiratory system more vulnerable to infection. Chronic health conditions—such as chronic obstructive pulmonary disease (COPD), diabetes, and heart ailments—further hamper the body’s ability to ward off pneumonia. Recognizing and addressing these pre-existing health issues is an important foundation for any prevention strategy in older Australians.
Lifestyle and living environment can also play a pivotal role in risk dynamics. Seniors residing in aged care facilities face a higher incidence of respiratory infections compared to those living independently. Shared spaces, exposure to multiple caregivers, and the potential for longer-term exposure to influenza viruses or bacteria create a more conducive setting for pneumonia to spread. Regular evaluation of infection control practices in these settings is therefore critical.
The influence of seasonal trends is pronounced in Australia. Studies have consistently shown an uptick in pneumonia cases during the colder months, especially in the southern states. This surge is partly attributed to increased indoor gatherings and circulation of respiratory viruses. Seniors should be particularly vigilant during this period, with healthcare providers taking proactive steps to identify vulnerable individuals before winter peaks.
Socioeconomic factors cannot be overlooked. Access to preventive care and educational resources about pneumonia is not always uniform across Australia’s regions. Rural and remote communities may face particular barriers, both in terms of healthcare availability and public health messaging. Organizations like the Lung Foundation Australia have sought to bridge these gaps through outreach and telephone support initiatives tailored to high-risk groups.
Vaccination is a proven cornerstone of pneumonia prevention in the Australian senior population. The pneumococcal vaccine, alongside yearly influenza immunizations, dramatically reduces the risk of severe illness. National recommendations urge everyone over 65 to maintain up-to-date vaccinations, with the National Immunisation Program providing guidance and subsidies to make implementation easier.

Promoting good respiratory hygiene is equally crucial for this age group. Handwashing, mask use during illness outbreaks, and avoiding crowded indoor settings when possible all help limit exposure. Caregivers and family members play a frontline role in modeling and reinforcing these habits, especially when assisting seniors who may have diminished mobility or cognitive challenges.
Regular medical check-ups allow for early identification of risk factors and prompt intervention if symptoms appear. Australian general practitioners (GPs) are trained to recognize subtle indications of pneumonia unique to seniors, such as sudden confusion or a decline in physical function. Quick referrals to respiratory clinics or relevant specialists empower families to initiate care before complications arise.
Community-based initiatives, from informational workshops to telehealth check-ins, extend preventive care beyond the clinic. Programs run by organizations like Healthdirect Australia provide seniors and their support networks with easy access to accurate information and timely advice, ensuring a broad safety net across both urban centres and remote communities.
Effective pneumonia care begins with prompt diagnosis and continuous monitoring, especially for seniors whose illness may progress rapidly. Hospitalizations are common among Australians over 70, making discharge planning and post-hospital follow-up vital. Hospitals often coordinate with community nurses to ensure seniors return home to a supportive, well-informed environment where treatment regimens are followed meticulously.

Rest and hydration remain foundational, but care plans are increasingly individualized. In some cases, rehabilitation specialists work with patients to restore mobility and lung capacity post-infection. This approach not only accelerates physical recovery but also reduces the likelihood of re-admission for pneumonia or related complications.
Medication management can be complex for older Australians, who may already be on numerous prescriptions. Healthcare teams attentively monitor for interactions and adjust antibiotics or supportive drugs as required. Families are encouraged to maintain medication schedules and watch for any signs of side effects or deteriorating conditions, reporting concerns promptly to the care team.
Peer and caregiver support is a critical, if sometimes overlooked, element of the recovery process. Accessing advice from trusted sources like Lung Foundation Australia and community support groups increases confidence and competence among both patients and their loved ones. Such networks allow families to share best practices and emotional support throughout the recovery trajectory.
Recent years have witnessed considerable shifts in how pneumonia is managed among older adults in Australia. Telehealth advancements, introduced widely during the COVID-19 pandemic, are now integrated into routine care for at-risk seniors. These virtual consultations reduce the need for unnecessary clinic visits while keeping health professionals closely connected to vulnerable populations, especially in rural areas.

There is also growing recognition of the role of multidisciplinary teams. Respiratory nurses, dietitians, physiotherapists, and geriatricians collaborate for comprehensive, whole-person care—addressing nutritional needs, mobility challenges, and mental health alongside respiratory symptoms. This holistic approach is especially beneficial for seniors with complex health profiles.
Data-driven public health initiatives now leverage real-time surveillance of respiratory illness trends, allowing for targeted interventions ahead of seasonal spikes in pneumonia. These efforts, championed by both government agencies and not-for-profits, have led to more rapid information dissemination and efficient allocation of preventive resources such as vaccine clinics and outreach services.
Looking forward, the focus in Australia continues to shift toward proactive risk minimization and individualized support, reducing the broad impact of pneumonia on an aging population. By staying informed and prepared, families and caregivers can contribute to improved health outcomes for seniors, benefitting communities across the country.